TMJ Pain and TMD Treatment in Melbourne CBD
Evidence-informed care for jaw pain, clicking, headaches and facial tension.
If you’re experiencing jaw pain, clicking, headaches or ear symptoms, temporomandibular disorder (TMD) may be contributing. At The Headache and Neck Pain Clinic we provide personalised TMJ assessments and care for people in Melbourne CBD and surrounding areas, focusing on the underlying causes — not just symptom relief.

Why Does TMJ Pain Develop?
TMJ pain and temporomandibular disorder (TMD) often develop when the muscles, joints and discs that control your jaw stop working smoothly together.
Because all of the muscles that stabilise and move your jaw attach to your head and neck, problems in these areas commonly affect jaw function. Head or neck injuries, prolonged postures, or dental changes can all play a role.
One of the most common contributors we see in our Melbourne CBD clinic is prolonged forward-head posture, such as slumping at a desk or working on a laptop for long periods. This posture stretches the muscles connecting your neck to your jaw, gradually restricting normal jaw movement.
TMJ pain may also develop after:
- Trauma to the jaw or face
- Whiplash injuries (over 20% of people with whiplash develop TMD)
- Bite misalignment or malocclusion
- Long dental appointments with the mouth held open
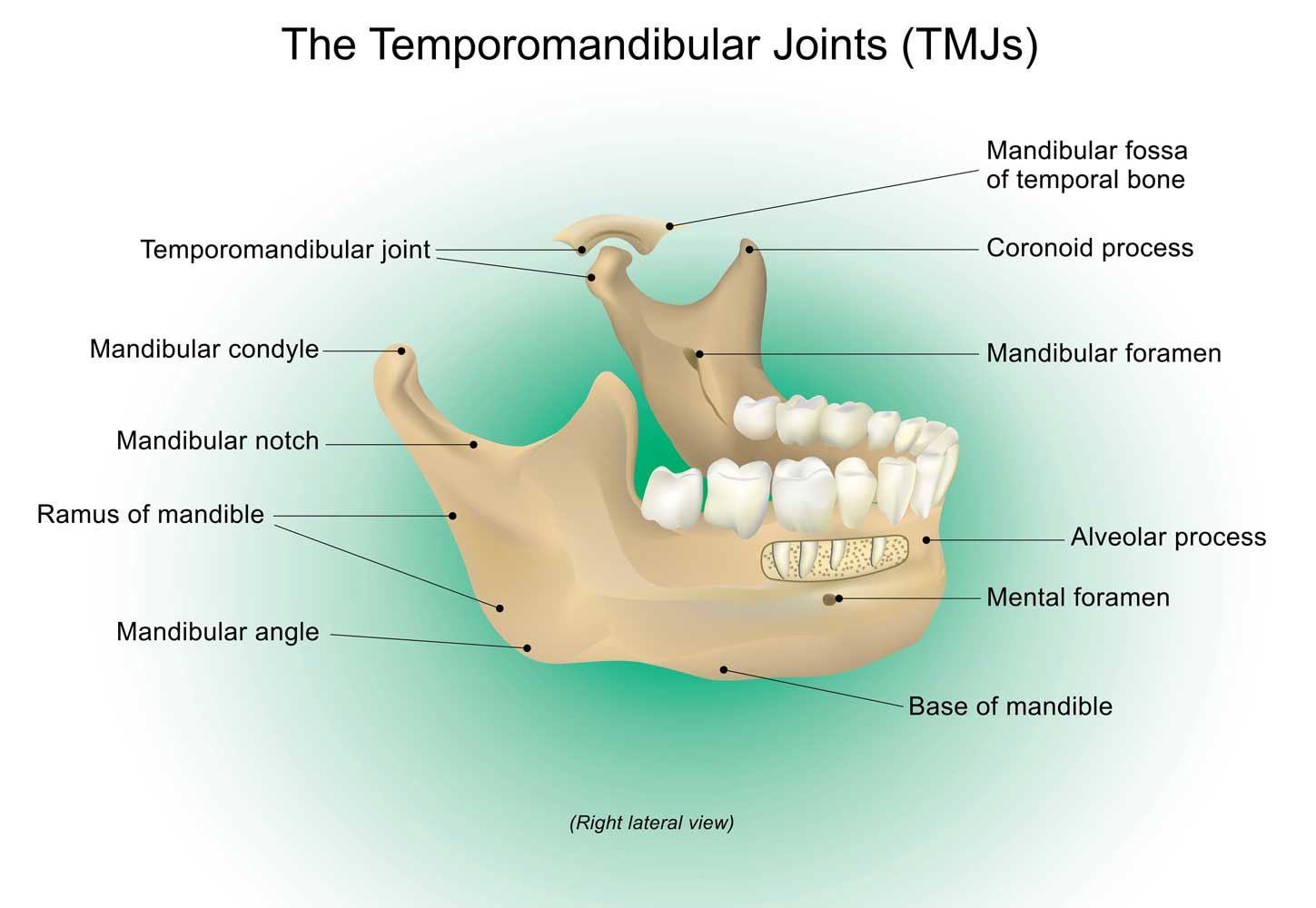
The temporomandibular joints are the most complex joints in the body. They rely on precise coordination between muscles, ligaments and small discs to allow smooth opening, closing and side-to-side movement.
What are the Signs and Symptoms of TMJ Pain and Dysfunction?
When jaw movement becomes restricted or uncoordinated, strain builds over time. This may lead to:
- Jaw pain or stiffness
- Clicking or popping sounds
- Fatigue when chewing
- Difficulty opening your mouth fully
- Locking or catching of the jaw
Clicking often occurs when the jaw slips off its disc during opening (disc displacement). If the disc returns when closing, this is called disc displacement with reduction. If it doesn’t, the jaw may lock (disc displacement without reduction), causing pain and limited movement.
TMJ dysfunction can also affect areas beyond the jaw. The TMJs share the trigeminal nerve with the teeth, ears, face and temples. Because of this, TMD may:
- Mimic dental pain or earache
- Trigger headaches
- Contribute to tinnitus, dizziness or ear fullness
People with frequent headaches are significantly more likely to experience TMD:
- Tension headaches → 3× more likely
- Migraines → 10× more likely
- Research also shows that 87% of people with TMD experience ear-related symptoms
How is TMJ Pain and Dysfunction Assessed and Treated at The Headache and Neck Pain Clinic?
TMJ pain responds best when treatment focuses on why the problem developed, not just where it hurts. At The Headache and Neck Pain Clinic, TMJ assessments include:
- Jaw movement and coordination
- Neck posture and mobility
- Muscle tension and overuse
- Disc function
- Contributing habits such as clenching or grinding
You’ll be given a clear diagnosis:
- Myogenic TMD (muscle-driven — most common)
- Mixed TMD (muscle and joint involvement)
- Arthrogenic TMD (joint-driven — least common)
Your care plan is tailored to your comfort and goals. If manipulation isn’t appropriate for you, alternative techniques are always available.
Research shows that TMD responds well to manual therapy and exercise, including:
- Mobilisation or gentle manipulation
- Soft tissue therapy
- Dry needling
- Muscle energy and neuromuscular techniques
- Targeted exercises and posture support
These approaches aim to:
- Reduce muscle tension
- Restore smooth, coordinated jaw movement
- Improve neck and jaw stability
- Reduce the risk of recurrence
TMD can also affect sleep, mood and concentration. Research shows higher levels of anxiety, depression and poor sleep in people with chronic TMD. Your care plan considers these whole-person factors.
Some people feel improvement within a few sessions. Others — particularly when symptoms have been present for longer — may need 6–12 weeks. While there are no quick fixes, lasting improvement is achievable with the right approach.
TMJ Treatment for Melbourne CBD and Surrounding Areas
If you’re looking for personalised TMJ support in Melbourne CBD, a thorough assessment can help identify what’s driving your symptoms and guide a plan toward long-term relief.
👉 Book Your TMJ Assessment at The Headache and Neck Pain Clinic today:
Book an appointment online or call The Headache and Neck Pain Clinic.